1979
Let’s talk about suicide.
Depression can affect anyone. After musicians Chris Cornell and Chester Bennington died, I had their songs on constant repeat for days on end. I was born in 1979 and basically grew up with their music, along with that of the Smashing Pumpkins. As the Smashing Pumpkins is one of the few bands still alive and well, I’m celebrating with several references to their music in this post. Recently, chef Anthony Bourdain & designer Kate Spade killed themselves and my social media feed was filled with messages honoring their memories.
However, I also noticed many comments expressing confusion over why celebrities with everything end their lives. When a close friend of mine committed suicide almost ten years ago, the online criticism from strangers were merciless, condemning him for feeling sad enough to kill himself despite small children dying of cancer. I wonder if these trolls realise that people who commit suicide aren’t just having a bad day. They may not have a perspective that allows them to compare their apparent lives of abundance to sick kids’. Because they are themselves sick from an illness known as depression.
When is sadness actually depression?
Healthy people may experience transient sadness following loss or setbacks. When the sadness is prolonged, profound and pervasive, it may suggest a depressive disorder. Early symptoms of depressive disorder are low mood, loss of energy, poor sleep, poor appetite and loss of interest in activities. While people with mild depressive disorder can still continue vocational function, those with moderate to severe disorder cannot. They may have marked lethargy, poor concentration, inability to work and increased suicidal tendency.
In the Singapore National Mental Health Survey done 2 decades ago, the prevalence of depressive disorder in the adult population was estimated to be at 8%. Precipitating problems included family or relationship conflicts and work stress. Since early detection and treatment can lead to quick recovery and prevent suicidal behaviour, we must do better in detecting depression which can happen to anyone, including young people who seem to have it all. For elderly people, increasing frailty due to physical illnesses, loss of independent living and loneliness are risk factors. https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1479-8301.2003.00013.x
Try, Try, Try
What can I do as an emergency physician?
In the emergency department, many patients who might have depression come seeking for help but for other conditions, like a chronic headache or chest pain, or a plethora of symptoms that don’t add up to any specific identifiable physical cause. Mostly I think doctors are relieved for the patient’s sake that his symptoms are not due to a life or limb-threatening condition, but then we fail to address to underlying issue which may be psychological. Truthfully, most of us don’t remember too many details from our psychiatric training in medical school, including how to pick up clinical depression and the tools used by qualified psychiatrists are too complex. Yet we must try.
How do I diagnose depression?
Dr Doug Rund, an emergency physician, developed a bedside depression screening tool, “In SAD CAGES“, which stands for:
Loss of Interest in activities, Sleep disturbance, Appetite change, Depressed mood, Difficulty in Concentrating, Activity level change, Excessive Guilt, Loss of Energy, Suicidal thoughts, plans or attempt.
To screen positive for depression, the patient must have at least 5 out of the above 9 criteria on a daily basis for at least 2 weeks, including either loss of interest in activities or depressed mood. Several studies, including one done by Dr David Hoyer, show that the prevalence rates of depression in ED patients range from 20-30%.
How do I treat depression?
So the next challenge to emergency physicians is, what do we do with patients whom we have diagnosed with possible depression? Dr Hoyer believes in starting treatment with antidepressants from the ED. However many emergency physicians would prefer to refer such patients to a psychiatrist for initiation of treatment as some antidepressants have side effects. I think we can still try to help our patients, maybe with non-pharmacological methods while awaiting follow-up or even admission, to expedite team-based treatment especially if the patient has active suicidal ideation.
Infinite Sadness
When the doctor is unwell.
Hang on a minute. Based on the In Sad Cages screening tool, I myself might have skated on the edge of depression once or twice. Recently in the aftermath of some drama, I was beyond blue for a couple of weeks and checked enough boxes to be considered someone with possible depression. Even my nurses noticed and one left a coffee on my desk with the words, “Cheer up, okay? Smile, Dr Jade!”
What not to say.
While I have since bounced back, I’ll share with you what made me feel worse and held me back when I was trying to recover. Quite frankly, sometimes I regretted sharing about what I was sad about, because I might get a response like, “But, I think you allow yourself to feel sad,” or “You know, I think you’re making yourself feeling victimised, so don’t.” At that time, I found these remarks quite upsetting, and now as I recall them, I still find them quite patronising, if not damaging. Instead I found that when friends acknowledged that I was upset by certain circumstances, even if they didn’t take sides on the matter, I felt that I had been heard and believed. And that cleared my mind to pivot and come up with constructive solutions.
Tonight, Tonight
Searching for resolution.
How did I recover? To be honest, it was pretty difficult. I searched many avenues using time and money to obtain peace, but the more I pushed myself, the worse I felt. One day I felt like my body was breaking down. I had rubbed my eyes until they were completely swollen, my skin was a curious mix of aged wrinkles & hormonal zits and my mood was on the floor. I was so blue I actually missed the yoga session I had planned for my own therapy.
Call for help.
Eventually I just called a friend and we went for a long walk. We followed our feet with a vague idea to visit a couple of bars along the way. From a rooftop bar at Fraser Road, we saw some parachuters jump out of planes in preparation for the National Day Parade next month. When we crossed the street at City Hall to make our way to the bay, fighter jets zipped over us. As we passed the Esplanade, we found an urban playground hidden in plain sight. Delighted, we filled our instastories with videos of kids laughing happily, old boats crossing the Fullerton Bay and the padparascha sunset in all his variegated glory as he blushed across the sky. Tourist game strong, we even snapped photos of the merlion.
Just breathe.
The biggest surprise was when we saw a phenomenal display of explosive fireworks as we sat at Cafe Fernet. As I watched the dust settle in the sudden silence, I breathed intentionally. I felt a quiet sense of calm and released my negative feelings to God and His universe. I couldn’t help but wonder at how our spontaneous walk had led us to this spot. Here I was tonight in the right spot at the right time to catch that stunning spectacle and find healing.
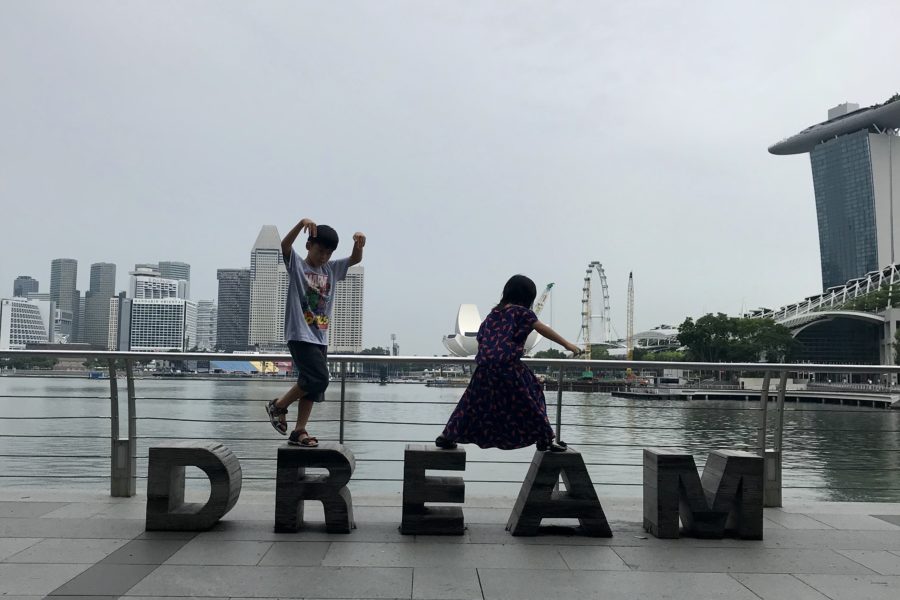
The Beginning Is the End Is The Beginning
Funnily enough, the next day, M1 whose friend from boarding school was visiting Singapore, asked if we could have lunch at Marina Bay Sands, in order to show his visitor around. After lunch the big boys scurried off to the airport, leaving me with M4 and M5. We wandered around and before I knew it, I was back in the same area as I was the night before. And in the clear light of day with my kids scampering over signs that spelt DREAM as they danced to singing buskers, I was glad I was in the same good place, grounded by my feet, but also in the same good space, in my heart & mind.
References:
Fones C, Kua EH, Ko SM, Ng TP. Studying the mental health of a nation. Singapore Medical Journal 1998; 9:251-255.
Kua EH. A community study of mental disorders in elderly Singaporean Chinese using the GMS-AGECAT package. Australian and New Zealand Journal of Psychiatry 1992; 26:502-506.
Rund DA. Behavioral disorders: clinical features. In: Tintinalli JE, Kelen GD, Stapczynski JS, ed. Emergency medicine, a comprehensive study guide, 6th edn. Irving, TX: American College of Emergency Physicians; 2004:1810.
Hoyer D, David E. Screening for depression in emergency department patients. J Emerg Med. 2008 Nov 18.
Kumar A, Clark S, Boudreaux ED, Camargo CA. A multicenter study of depression among emergency department patients. Acad Emerg Med. 2004;11:1284-1289.
Screenshots from Instagram used in spirit as intended by original source, with thanks to @mzsharonlim @russelwong @katespadeny @eleventhour.

















6 Comments
Leave your reply.